Unit 9 – Vitamins and Minerals Part 2
9.2 Introduction to Bone Health
The human skeleton consists of 206 bones and other connective tissues that together support and protect many organs, produce red and white blood cells, and act as a storage depot for minerals such as calcium, phosphorus, and magnesium. Although bones may look inactive at first glance, they are living tissues that are dynamic and in a constant state of breaking down and rebuilding to withstand mechanical forces. Bones also contain a complex network of canals, blood vessels, and nerves that allow for nutrient transport and communication with other organ systems.
Nutrition influences all body systems, and the skeletal system is no exception. Our lifestyle choices impact the health of our bones. In this section, we will look at how bone forms across the lifecycle and discuss the complex interactions of nutrients, hormones, genetics, and environmental factors that impact bone health.
What Is Bone?
Bone is a living tissue made of proteins and minerals. The proteins, like collagen, provide the soft framework for bones, and the inorganic minerals harden the collagen framework and provide strength. The combination of collagen and minerals makes bone both flexible and strong, which allows it to withstand stress.
Most bones contain two types of tissue, compact and spongy tissue. Spongy bone (also known as trabecular bone) is 50 to 90 percent porous and appears lattice-like under a microscope. Compact bone (also known as cortical bone) is dense to withstand compressive forces. It is only 10 percent porous and looks similar to the rings in a tree trunk, with many concentric circles sandwiched together. Compact bone tissue makes up approximately 80 percent of the adult skeleton and surrounds all spongy tissue.
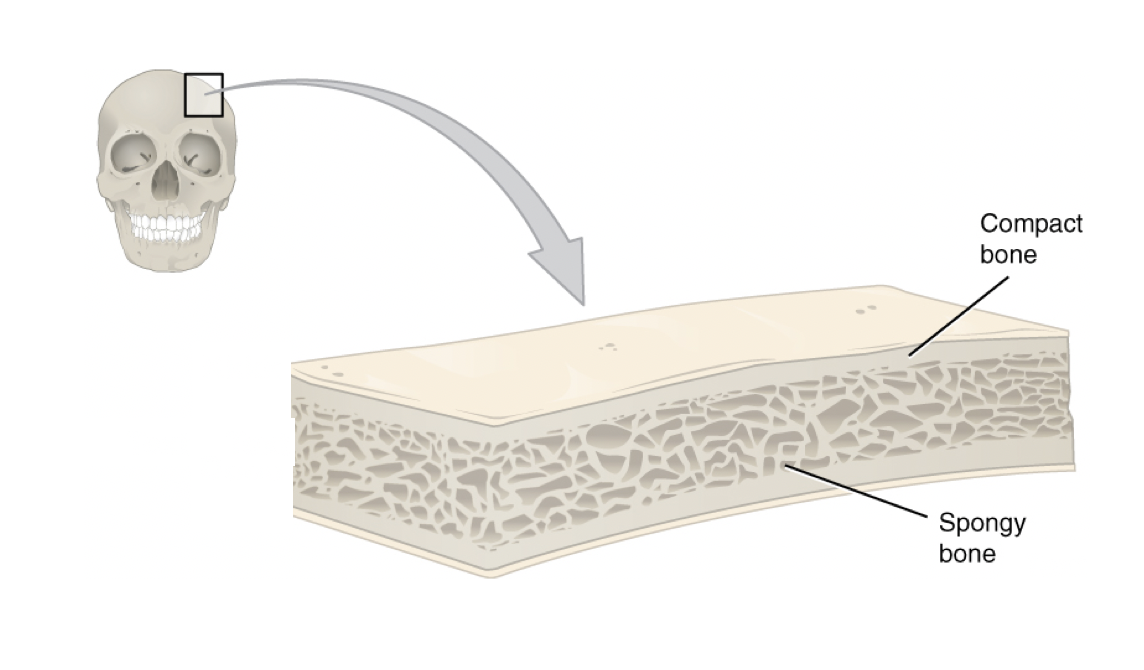
Figure 9.1. This cross-section of a flat bone from the skull shows the spongy bone lined on either side by a layer of compact bone.
Bone Growth, Modeling, and Remodeling
Bones change in shape, size, and position throughout the life cycle. During infancy, childhood, and adolescence, bones continuously grow and shape through two processes: growth (or ossification) and modeling. In the modeling process, bone tissue is dismantled at one site and built up at a different site, which influences the shape of the bone. During childhood and adolescence, more bone is deposited than dismantled, so bones grow in size and density, reaching 90 percent of peak bone mass by age 18 in girls and 20 in boys.2 Peak bone mass is reached by age 30, at which point bones have reached their maximum strength and density. Factors affecting peak bone mass include sex, race, hormones (e.g., estrogen and testosterone), nutrition (e.g., calcium and vitamin D intake), physical activity, and behavioral factors like smoking. These factors will be discussed in more detail when we discuss osteoporosis.
In adulthood, our bones stop growing and modeling, but they continue to undergo a process of bone remodeling, in which bone tissue is degraded and built up at the same location. About 10 percent of bone tissue is remodeled each year in adults. Bones adapt their structure to the forces acting upon them, even in adulthood. This is why physical activity increases bone strength, especially in weight-bearing activities. For example, tennis players can have measurably higher bone mass in the arm they use for play compared with the other arm.3 Ultimately, bones adapt their shape and size to accommodate function.
The decline in bone mass after age 40 occurs because the rate of bone loss is greater than the bone formation rate. As we’ll discuss next, how much bone is lost in adulthood depends on the peak bone mass reached in early adulthood and other risk factors.
Osteoporosis
Osteoporosis is a bone disease that occurs when bone density or bone mass decreases. The bone becomes thinner and more porous, therefore more susceptible to breaking. More than 53 million people in the U.S. either have osteoporosis already or are at high risk of developing it due to low bone mass.1
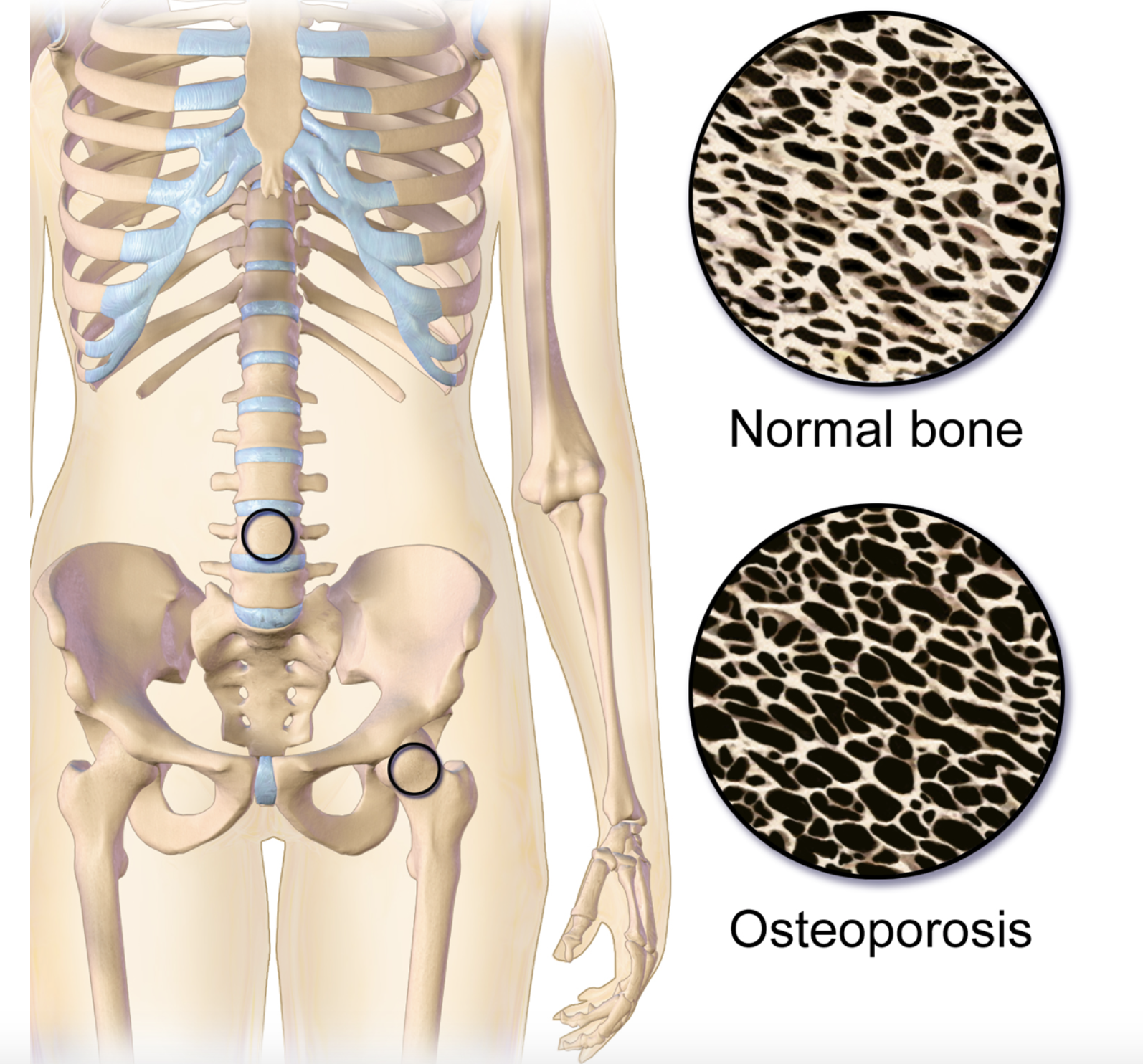
Figure 9.2. Osteoporosis. This illustration shows the difference between the structure of normal bone, which is less porous, and bone with osteoporosis, which is more porous. The two circles located on the spine and hip represent the location of the images.
Bone loss usually occurs without symptoms, so osteoporosis is often called a silent disease. It can go undetected until bones become so weak that they fracture due to a sudden strain, bump, or fall.
An individual’s chances of developing osteoporosis depend on several risk factors, some of which are controllable and some of which are not. It is thought that genetic factors (such as sex and race) may account for up to 75 percent of bone mass, and lifestyle factors (such as diet and exercise habits) account for the remaining 25 percent.2
Osteoporosis risk factors that are biological and can’t be controlled:
- Body frame size- People with small frames are at higher risk for osteoporosis.
- Race- Caucasian and Asian populations are at higher risk of osteoporosis compared to African American and Hispanic populations, which are at lower risk.1
- Family history– Having a family member with osteoporosis may increase risk, as heredity seems to play a part in the development of osteoporosis.
- Age- After age 40, bone mass declines due to bone breakdown exceeding bone formation. Therefore, any person over 40 is more likely to develop osteoporosis than a younger person. Starting out with a higher peak bone mass in early adulthood allows you to lose less bone during aging and not develop osteoporosis.
- Sex- Females, on average, have a lower peak bone mass compared with males (see Figure 9.3) and a much greater risk of developing osteoporosis, partly because of hormone levels.
- Hormones- The female hormone estrogen and the male hormone testosterone both help to increase peak bone mass. Estrogen is the primary female reproductive hormone, stimulating bone building and reducing bone breakdown. When women go through menopause (usually around age 50), they experience a natural decline in estrogen levels, which accelerates bone loss and increases the risk of developing osteoporosis (Figure 9.3).
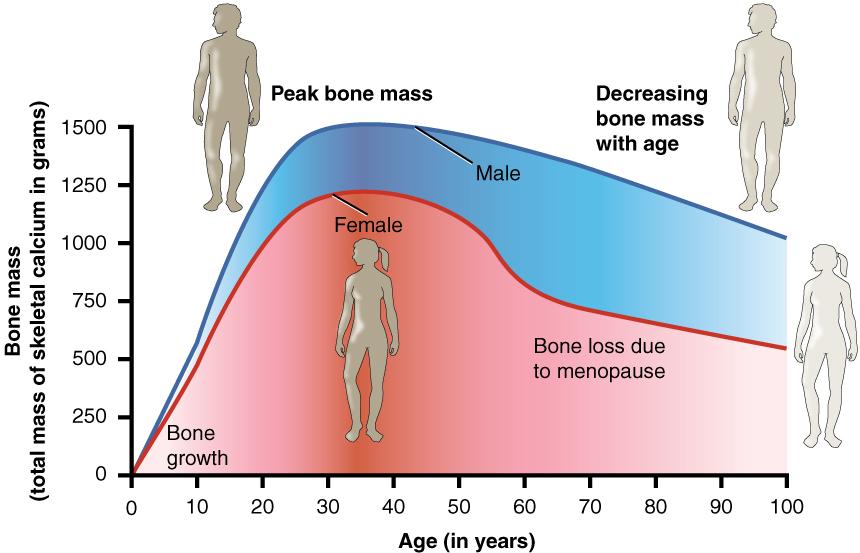
Figure 9.3. Age and bone mass. Bone density peaks at about 30 years of age, and women lose bone mass more rapidly than men, particularly around menopause.
Risk factors that can be controlled:
- Physical inactivity- Physical inactivity lowers peak bone mass, decreases BMD at all ages, and is linked to increased fracture risk, especially in the elderly. Regular exercise can help individuals achieve greater peak bone mass, prevent bone loss in women and men aged 30 and older, and maintain strength and balance to help prevent falls later in life. The best activities for stimulating new bone are weight-bearing exercises like walking, hiking, and dancing, and resistance exercises like weight lifting.
- Nutrition- Ensuring adequate nutrition is a key component in maintaining bone health. Having low dietary intakes of calcium and vitamin D is a strong risk factor for developing osteoporosis. Protein is also important during childhood and adolescence for proper bone development and in older age to preserve bone mass.4
- Smoking- Smoking cigarettes has long been known to correlate with a decrease in bone mass and an increased risk of osteoporosis and fractures. However, because people who smoke are more likely to be physically inactive and have poor diets, it is difficult to determine whether smoking itself causes osteoporosis. Smoking is also linked to earlier menopause. Therefore, the increased risk of developing osteoporosis among female smokers may also be attributed, at least partly, to reduced estrogen production at an earlier age. However, studies have also shown that tobacco smoke and nicotine can directly impact bone metabolism.5
- Alcohol intake- Alcohol intake may also affect bone health, although this seems to depend on the amount consumed. Light alcohol intake (one 1 drink or less per day) has been shown in some studies to be associated with increased bone density and a decreased risk of developing osteoporosis. However, excessive alcohol intake is associated with decreased bone density and increased fracture risk, although this may be due in part to other lifestyle factors, such as poor diet and less physical activity. 6
- Being underweight- Being underweight significantly increases the risk of developing osteoporosis because underweight people often have a smaller frame size and a lower peak bone mass. The most striking relationship between being underweight and bone health is seen in people with anorexia nervosa. Anorexia nervosa is strongly correlated with low peak bone mass, and more than 50 percent of men and women who have this illness develop osteoporosis, often very early in life.
The changeable risk factors for osteoporosis provide ways for people to improve their bone health, even though some people may be genetically predisposed to the disease. Prevention of osteoporosis begins early in life since this is a critical time of bone growth. Eating a balanced diet that provides adequate amounts of calcium, vitamin D, and protein is important for bone health throughout the life cycle. Participating in exercises such as walking, hiking, and weight lifting, and refraining from risky behaviors like smoking and excessive drinking are all behaviors that will help protect bones.
Self-Check:
Attributions:
- Lane Community College’s Nutrition: Science and Everyday Application CC BY-NC.4.0
References:
- 1National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis Overview. Retrieved April 22, 2020 from https://www.bones.nih.gov/health-info/bone/osteoporosis/overview
- 2National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis: Peak Bone Mass in Women. Retrieved April 22, 2020 from https://www.bones.nih.gov/health-info/bone/osteoporosis/bone-mass
- 3Kontulainen S., Sievanen H., Kannus P., Pasanen M., Vuori I. (2002). Effect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controls. J Bone Miner Res 17: 2281–2289.
- 4International Osteoporosis Foundation. Nutrition. Retrieved April 28, 2020 from https://www.iofbonehealth.org/nutrition
- 5Al-Bashaireh, A. M., Haddad, L. G., Weaver, M., Chengguo, X., Kelly, D. L., & Yoon, S. (2018). The Effect of Tobacco Smoking on Bone Mass: An Overview of Pathophysiologic Mechanisms. Journal of osteoporosis, 2018, 1206235. https://doi.org/10.1155/2018/1206235
- 6Gaddini, G. W., Turner, R. T., Grant, K. A., & Iwaniec, U. T. (2016). Alcohol: A Simple Nutrient with Complex Actions on Bone in the Adult Skeleton. Alcoholism, clinical and experimental research, 40(4), 657–671. https://doi.org/10.1111/acer.13000
- Images:
- Figure 9.1. “Anatomy of a Flat Bone” by J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix, Anatomy and Physiology, OpenStax, licensed under CC BY 4.0
- Figure 9.2. “Osteoporosis” by BruceBlaus is licensed under CC BY-SA
- Figure 9.3. “Age and bone mass” by Anatomy & Physiology, Connexions Web site is licensed under CC BY 3.0

