Unit 7- Energy Balance and Obesity
7.6 Weight Loss Strategies
We have just considered the gravity of the obesity problem. This section explores various weight loss strategies and the effectiveness of each. Successful weight-loss is when a person intentionally loses at least 10 percent of his body weight and keeps it off for at least a year.3 Results from studies suggest that most of us are not successful. A large-scale study involving more than 14,000 adults found that only one in six overweight or obese individuals were able to lose weight and keep it off for one year.4 This raises the question: Why is achieving long-term weight loss so difficult? Much of the explanation lies in understanding the biology of weight loss.
Biology of Weight Loss
As discussed earlier, if you eat more calories than you burn, you gain weight. If you burn more calories than you eat, you lose weight. This general formula of energy balance gives foundation to the basic premise of weight management.
However, the body is more complex than a simple formula. And like other functions within the body, weight is tightly regulated. To prevent perpetual weight loss or weight gain, our bodies strive to keep weight at a constant point.5 But our obesogenic environment often promotes behaviors that encourage excessive caloric intake and lower energy expenditure, leading to weight gain over time.
At the start of a weight loss diet, we typically drop pounds rapidly. But the same mechanisms that work to maintain a steady weight also kick in during periods of weight loss to help us maintain our original weight.5 The body recognizes weight loss as a threat to survival, lowering basal metabolic rate to preserve calories and protect against starvation. Additionally, as body weight decreases, we need less energy to carry our lighter body weight. This results in fewer calories burned through physical activity.
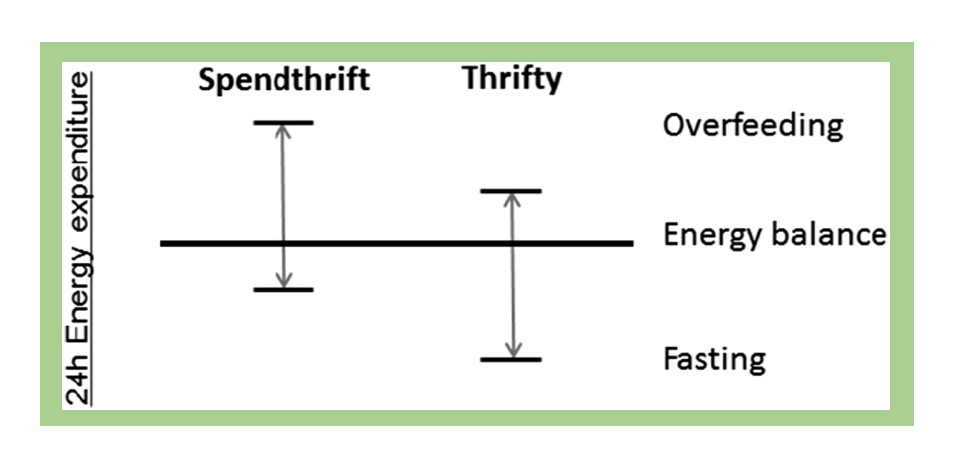
Biological differences in individual metabolism may also impact weight loss success. Researchers have found that some individuals have a “thrifty” metabolism, meaning that they have a lower metabolic rate. These thrifty individuals expend fewer calories when in a fasting (or calorie-restricted) state, common in weight loss efforts. This results in a lower level of weight loss. In contrast, individuals with a “spendthrift” metabolism tend to have a higher metabolic rate in a fasting state, burning more calories and thus making weight loss easier.6 According to researcher Martin Reinhardt, “The results corroborate the idea that some people who are obese may have to work harder to lose weight due to metabolic differences.”7
Figure 7.23. Illustration of the concept of spendthrift and thrifty metabolisms, characterized by their response to overfeeding and fasting.
Research also suggests that changes in hormone levels due to weight loss may affect the body’s ability to keep the weight off. Thyroid hormone levels decrease, which lowers the metabolic rate. As fat cells decline, leptin levels also decline, increasing appetite and decreasing metabolic rate. These hormonal changes result in the need for fewer calories and makes keeping the weight off difficult.5,8 These biological factors and their influence on weight are discussed further in the below video.
VIDEO: “The Quest to Understand the Biology of Weight Loss,” by HBO Docs, YouTube (May 14, 2012), 22:52 minutes.
Components of Weight Loss Program
Evidence suggests that successful weight loss and maintenance are possible despite the challenges imposed by biological processes in our bodies. There are many approaches when considering options for weight loss, and no single treatment is suitable for everyone. The three components for weight loss include:
- Eating fewer calories (mainly fat and added sugars).
- Increasing physical activity.
- Incorporating behavioral modification.
Dietary Considerations for Weight Loss
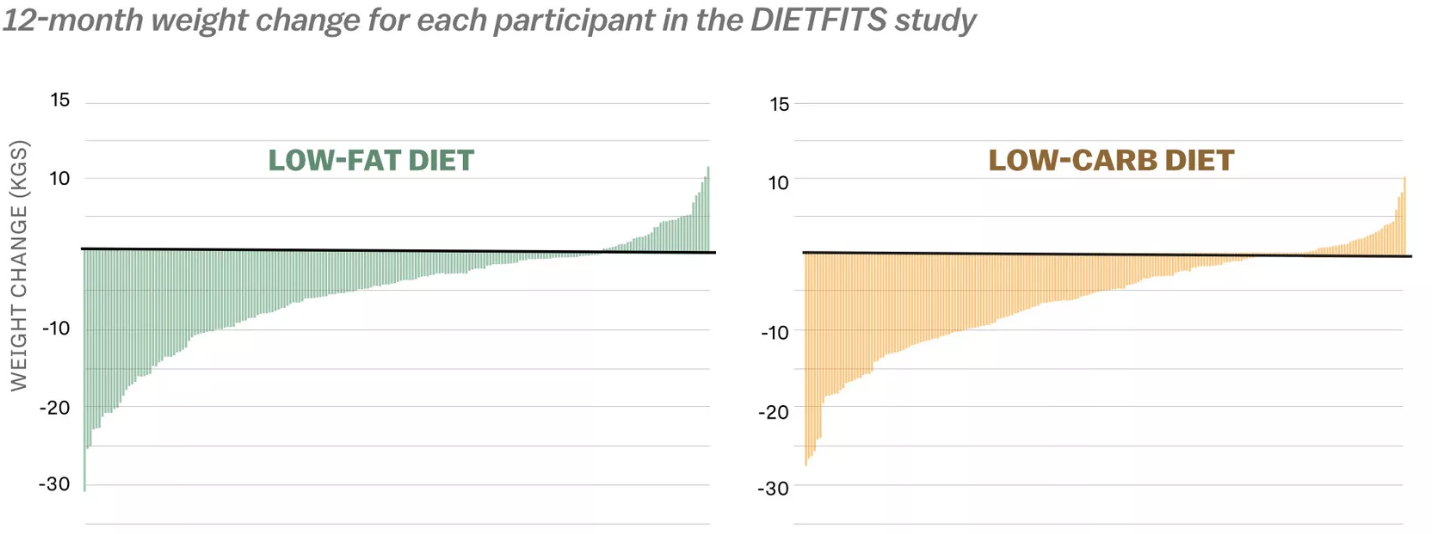
Although following a lower-calorie healthy eating plan is often the first approach to weight loss, research shows that no single dietary strategy is superior to others.9,10 For example, a recent trial, called the DIETFITS study, followed participants on either a low-fat or low-carbohydrate diet for one year and found no significant difference in weight loss between study groups. Both dietary strategies produced a range of weight loss results. Some participants lost more than 60 pounds, and others gained 20 pounds over the year, suggesting that what works for one individual may produce varying effects in others.1
Figure 7.24. Results from the DIETFITS study show that regardless of the type of diet followed, participants experienced a similar wide range of changes in weight.
To learn more about the DIETFITS study, check out the following video.
VIDEO: “Stanford’s Christopher Gardner Tackles the Low-Carb vs. Low-Fat Question.” by Stanford Medicine, YouTube (February 19, 2018), 4:08 minutes.
National Weight Control Registry
The National Weight Control Registry (NWCR) has tracked more than 10,000 people who have successfully lost 30 pounds and maintained this weight loss for at least one year. Their research findings show that 98 percent of participants in the registry modified their food intake, and 94 percent increased their physical activity, mainly by walking.11
There was a great variety of approaches taken by NWCR members to achieve successful weight loss. Most involved a low-calorie, low-fat diet while exercising. (Most got one hour of exercise per day.) Moreover, most members eat breakfast every day, watch fewer than ten hours of television per week, and weigh themselves at least once per week. About half of them lost weight independently, and the other half used some type of weight-loss program.
In most scientific studies, successful weight loss is accomplished only by changing the diet while increasing physical activity. Doing one without the other limits the amount of weight loss and the length of time that weight loss is sustained.12
Dietary Recommendations for Weight Loss
The 2020 Dietary Guidelines for Americans offers specific, evidence-based recommendations for dietary changes aimed at keeping calorie intake in balance with physical activity, which is key for weight management.13 These recommendations include following a healthy eating pattern that accounts for all foods and beverages within an appropriate calorie level, including the following:
- A variety of vegetables from all of the subgroups—dark green, red and orange, legumes (beans and peas), etc.
- Fruits, especially whole fruits
- Grains, at least half of which are whole grains
- Fat-free or low-fat dairy, including milk, yogurt, cheese, and/or fortified soy beverages
- A variety of protein foods, including seafood, lean meats and poultry, eggs, legumes (beans and peas), and nuts, seeds, and soy products
- Oils, including vegetable oils and oils in foods, such as seafood and nuts
A healthy eating pattern also limits several components of public health concern in the U.S.:
- Consume less than 10 percent of calories per day from added sugars
- Consume less than 10 percent of calories per day from saturated fats
- Consume less than 2,300 milligrams (mg) per day of sodium
- If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and up to two drinks per day for men—and only by adults of legal drinking age.
Typical Dietary Intakes of Americans
While these guidelines establish basic recommendations for dietary intake across all food groups, most Americans do not achieve these recommendations. Figure 9.26 shows how Americans are falling short in meeting the recommendations for vegetables, fruit, whole grains, dairy, and seafood and consume well over the recommended amount for refined grains. Meanwhile, many Americans also exceed the recommended added sugars, saturated fats, sodium, and alcohol limits. As recommended in the Dietary Guidelines, shifting towards more nutrient-dense choices would help balance caloric intake and meet nutrient needs for optimal health.
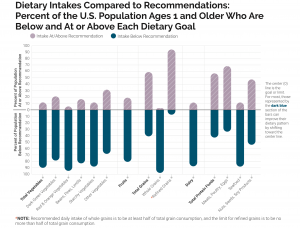
Figure 7.25. The percentage of the U.S. population ages 1 year and older with intakes below the recommendation or above the limit for different food groups and dietary components.
Physical Activity Recommendations For Weight Loss
Physical activity is a vital part of losing weight and keeping it off. The 2018 Physical Activity Guidelines for Americans provides recommendations to Americans aged three and older about improving health and reducing chronic disease risk through physical activity. Increased physical activity lowers the risk of heart disease, stroke, high blood pressure, Type 2 diabetes, colon, breast, lung cancer, falls and fractures, depression, and early death. Increased physical activity not only reduces disease risk but also improves overall health. Benefits include enhancing cardiovascular and muscular fitness, increasing bone density and strength, improving cognitive function, and losing weight and keeping it off.14
The key guidelines for teens and adults include the following:
- Move more and sit less throughout the day. Some physical activity is better than none. Teens and adults who sit less and do any amount of moderate-to-vigorous physical activity have improved health.
- Do at least 150 to 300 minutes per week of moderate-intensity aerobic activity, or 75 minutes to 150 minutes per week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity.
- Gain additional benefits by engaging in physical activity beyond the equivalent of 300 minutes of moderate-intensity physical activity per week. It may help with losing weight and keeping it off.
- Spread aerobic activity throughout the week.
- Do moderately-intense, muscle-strengthening activities that involve all major muscle groups on two or more days per week. Exercises such as push-ups, sit-ups, squats, and lifting weights are examples of muscle-strengthening activities. These activities provide additional health benefits.
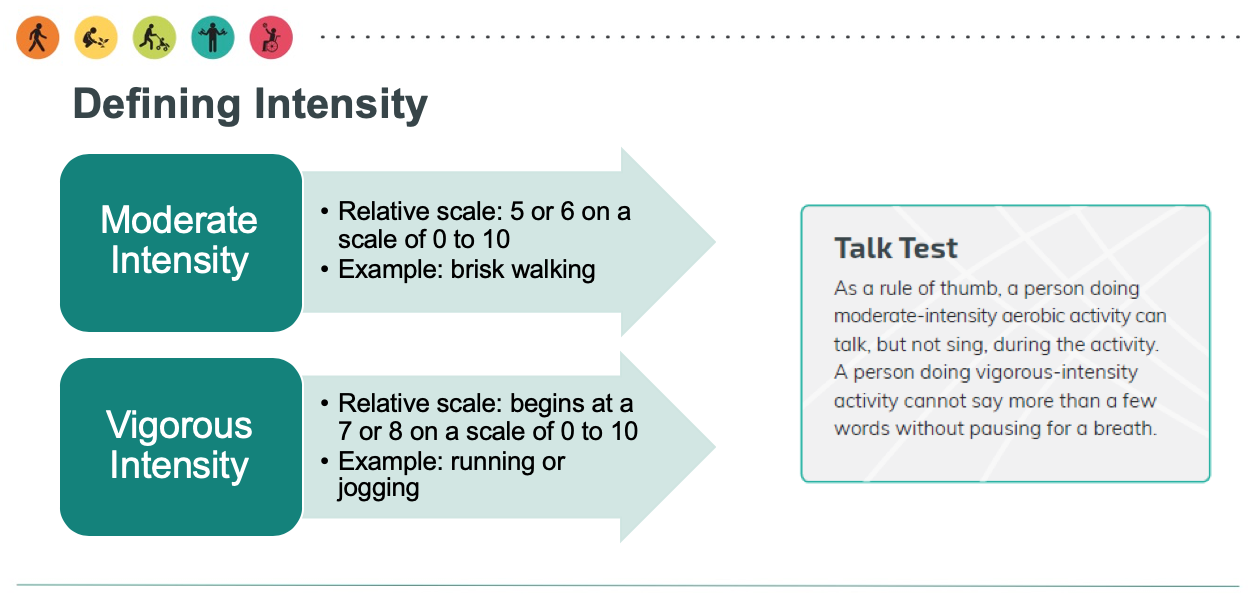
Moderate vs. Vigorous Activity
The 2018 Physical Activity Guidelines broadly classify moderate physical activities as those when you “can talk, but not sing, during the activity” and vigorous activities as those when you “cannot say more than a few words without pausing for a breath.”14 Despite the indisputable benefits of regular physical activity, a 2018 report from the American Heart Association estimates that 8 out of 10 Americans do not meet these guidelines.2
Figure 7.26. The 2018 Physical Activity Guidelines’ definition of moderate-intensity and vigorous-intensity exercise.
Given the number of Americans that are falling short on both nutrition and physical activity recommendations, it is easy to see that these two areas of behavior are of primary interest in improving the health and weight of our nation.
Behavioral Aspects of Weight Loss
In addition to diet and physical activity, the third aspect of a weight loss program is behavioral. Behavior modification includes recognizing when and why you do certain things. For example, determining why you eat a candy bar or drink a soda.Or why do you sit on the couch watching television instead of walking the dog? If you recognize that you eat candy and drink soda when it’s in plain sight on the kitchen counter, you should either not buy them or hide them in a locked cabinet. If you watch TV because your TV is in your bedroom, move the TV to another place. Behavioral weight-loss interventions help us develop skills to achieve a healthier weight and keep those pounds off. It’s more than deciding what to change; it’s identifying how to change.
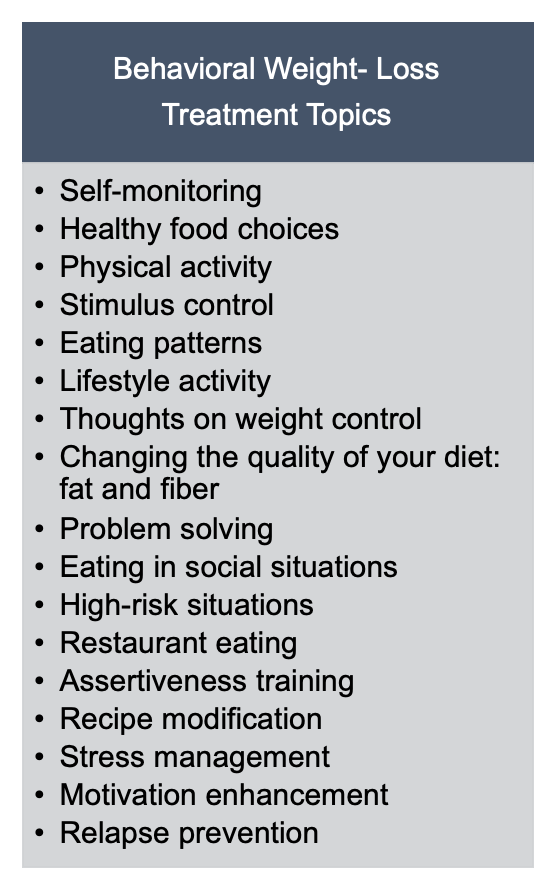
Cornerstones for behavior modification typically include keeping a daily recording of food intake and exercise. Additionally, nutrition education is combined with setting physical activity goals and behavior modification.16 Research shows that these interventions can result in weight loss and a lower risk for type 2 diabetes. Similar maintenance strategies lead to less weight regained later.17
Behavioral Health Team
The behavioral health team often includes primary care clinicians, dietitians, psychologists, behavioral therapists, exercise physiologists, and lifestyle coaches.17 These programs may consist of various delivery methods, often through group classes of 10-20 participants. The classes may be in-person or online courses and often use print and digital materials. The interventions usually span one to two years, with more frequent contact in the initial months (weekly to bi-monthly) followed by less regular contact (monthly) in the latter months or maintenance phase.17 A variety of behavioral topics are covered throughout the program and range from nutrition education and goal-setting to problem-solving and assertiveness. Relapse prevention is a part of the maintenance phase.16
Figure 7.27. Common topics included in behavioral interventions for weight loss, adapted from Smith, C. E., & Wing, R. R. (2000). New directions in behavioral weight-loss programs. Diabetes Spectrum, 13(3), 142-148.
Medically Prescribed Treatments
In some situations, diet, exercise, and behavior modification are not enough to lose weight. In these instances, health care providers may prescribe a medication (diet pill) that will suppress appetite or decrease the amount of fat absorbed. These medications should be used in conjunction with lifestyle changes and not in place. Individuals trying to lose weight should only use diet pills approved by the FDA for weight loss. 19 The FDA does not monitor over-the-counter weight loss supplements and does not recommend them for weight loss.
Bariatric surgery may be appropriate for individuals with a BMI over 40 or BMI over 35 with obesity-related coexisting conditions, so long as they’re motivated to lose weight and behavioral interventions (with or without medication) have not been effective. Potential candidates for surgery should be referred to an experienced bariatric surgeon for consultation and evaluation.19
Non-Diet Approaches to Weight Loss
In addition to weight management focusing on diet, exercise, and behavioral interventions, a growing movement centers around non-diet approaches. The trend is to have a healthier mentality toward food, weight, and body image. These approaches include establishing more beneficial relationships with food and more body acceptance and positivity regardless of shape and size. Many of these programs center around our relationship with food and making eating an enjoyable experience. The focus is on well-being rather than dieting. They do away with shame or guilt, often associated with failed weight loss efforts. They promote respect and inclusivity for all people regardless of weight or size. Mindful or intuitive eating are standard components of these approaches.
Small Change
“Small-Change” is a non-diet method to prevent weight gain. The approach, developed in 2003, promotes small lifestyle changes to reduce weight gain occurring over time. It may better reduce obesity rates in the American population in all age groups.[1] Currently, most people are not obese in this country. The gradual rise in overweight is happening because most eat slightly more calories than we burn. This combination results in a gradual weight gain of one to two pounds a year. A person can pack on 10 to 20 pounds in a decade, or 20 to 40 pounds from age 20 to 40 years.
Studies have demonstrated that using a pedometer to track the number of steps we take each day helps maintain a healthy weight. The 2007 “Small-Changes” study evaluated if families who walked an additional 2,000 steps and cut 100 kilocalories lost weight. One group of families tracked steps using a pedometer and replaced sugar with an artificial sweetener.[2] The results showed tracking steps with pedometers while cutting sugar promotes weight loss.[3] Several more studies funded by the National Institutes of Health and USDA are ongoing and evaluate the effectiveness of the “small-changes” approach in reducing weight gain. Time will tell if this approach is better than traditional weight loss diets.
Health at Every Size
Health at Every Size (HAES) is another movement started by the Association for Size Diversity and Health (ASDAH) organization as an alternative to weight-centered health models. HAES aims to decrease our culture’s obsession with body size and weight, decrease weight discrimination and stigma, and promote size acceptance and inclusivity.22 Key principles of the HAES approach include:
- Acceptance and respect for the inherent diversity of body shapes and sizes
- Health enhancement through policies and services that promote well-being in all aspects of health, including physical, economic, social, emotional, and spiritual needs
- Respectful care and elimination of weight bias and discrimination through proper education and training
- Eating behaviors are driven by hunger, satiety, nutritional needs, and pleasure instead of external regulation by diets and eating plans
- Physical activity through life-enhancing movement for all sizes and abilities
To learn more about non-dieting approaches for a healthy lifestyle, check out the following video.
VIDEO: “Why Dieting Doesn’t Usually Work,”from TED, 12:30 minutes.
Review Questions
Attributions:
- University of Hawai‘i at Mānoa Food Science and Human Nutrition Program, “Dietary, Behavioral, and Physical Activity Recommendations for Weight Management,” CC BY-NC 4.0
References:
- 1Obesity and overweight. Centers for Disease Control and Prevention. Retrieved November 13, 2019, from https://www.cdc.gov/nchs/fastats/obesity-overweight.htm.
- 2Han L, You D, Zeng F, et al. Trends in Self-perceived Weight Status, Weight Loss Attempts, and Weight Loss Strategies Among Adults in the United States, 1999-2006. (2019). JAMA Network Open. doi: https://doi.org/10.1001/jamanetworkopen.2019.15219
- 3Wing, R. R., & Hill, J. O. (2001). Successful weight loss maintenance. Annual review of nutrition, 21(1), 323-341.
- 4Kraschnewski, J. L., Boan, J., Esposito, J., Sherwood, N. E., Lehman, E. B., Kephart, D. K., & Sciamanna, C. N. (2010). Long-term weight loss maintenance in the United States. International journal of obesity, 34(11), 1644-1654. Retrieved November 8, 2019, from http://www.ncbi.nlm.nih.gov/pubmed/20479763.
- 5MacLean, P. S., Bergouignan, A., Cornier, M. A., & Jackman, M. R. (2011). Biology’s response to dieting: the impetus for weight regain. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 301(3), R581-R600. https://www.physiology.org/doi/full/10.1152/ajpregu.00755.2010.
- 6Reinhardt, M., Thearle, M. S., Ibrahim, M., Hohenadel, M. G., Bogardus, C., Krakoff, J., & Votruba, S. B. (2015). A human thrifty phenotype associated with less weight loss during caloric restriction. Diabetes, 64(8), 2859-2867. Retrieved November 11, 2019, from https://diabetes.diabetesjournals.org/content/64/8/2859.
- 7NIH/National Institute of Diabetes and Digestive and Kidney Diseases. (2015, May 11). Ease of weight loss influenced by individual biology. ScienceDaily. Retrieved November 11, 2019, from www.sciencedaily.com/releases/2015/05/150511162918.htm
- 8Rosenbaum, M., Kissileff, H. R., Mayer, L. E., Hirsch, J., & Leibel, R. L. (2010). Energy intake in weight-reduced humans. Brain research, 1350, 95-102. Retrieved November 11, 2019, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2926239/
- 9Treatment for overweight & obesity. National Institute of Diabetes and Digestive and Kidney Diseases.
Retrieved November 10, 2019, from
https://www.niddk.nih.gov/health-information/weight-management/adult-overweight-obesity/treatment. - 10Gardner, C. D., Trepanowski, J. F., Del Gobbo, L. C., Hauser, M. E., Rigdon, J., Ioannidis, J. P., … & King, A. C. (2018). Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. Jama, 319(7), 667-679. Retrieved November 13, 2019, from https://jamanetwork.com/journals/jama/fullarticle/2673150.
- 11Research Findings. The National Weight Control Registry. Retrieved November 8, 2019, from
http://www.nwcr.ws/Research/default.htm. - 12National Heart, Lung, Blood Institute, National Institute of Diabetes, Digestive, & Kidney Diseases (US). (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report (No. 98). National Heart, Lung, and Blood Institute.Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Heart, Lung, and Blood Institute. 51S–210S.
- 13U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary Guidelines for Americans, 2020-2025, 9th Edition. Retrieved from https://www.dietaryguidelines.gov/
- 142018 Physical Activity Guidelines for Americans. US Department of Health and Human Services. Retrieved November 11, 2019, from https://health.gov/paguidelines/second-edition/.
- 15Yanovski, S. (2017, December). The challenge of treating obesity and overweight: Proceedings of a workshop. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board. Roundtable on Obesity Solutions, Washington (DC). Retrieved November 13, 2019, from https://www.ncbi.nlm.nih.gov/books/NBK475856/.
- 16Smith, C. E., & Wing, R. R. (2000). New directions in behavioral weight-loss programs. Diabetes Spectrum, 13(3), 142-148. Retrieved November 13, 2019, from http://journal.diabetes.org/diabetesspectrum/00v13n3/pg142.htm.
- 17Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., … & Kubik, M. (2018). Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US preventive services task force recommendation statement. JAMA, 320(11), 1163-1171.
- 18Donnelly, J. E., Blair, S. N., Jakicic, J. M., Manore, M. M., Rankin, J. W., & Smith, B. K. (2009). Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise, 41(2), 459-471.
- 19Jensen, M. D., Ryan, D. H., Apovian, C. M., Ard, J. D., Comuzzie, A. G., Donato, K. A., … & Loria, C. M. (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology, 63(25 Part B), 2985-3023.
- 20Satter, E. (2007). Eating competence: Nutrition education with the Satter eating competence model. Journal of Nutrition Education and Behavior, 39(5), S189-S194. Retrieved November 12, 2019, from
https://www.jneb.org/article/S1499-4046(07)00467-8/abstract. - 21The Satter Eating Competence Model. Retrieved November 10, 2019, from
https://www.ellynsatterinstitute.org/satter-eating-competence-model/. - 22The Health at Every Size Approach. Association for Size Diversity and Health. Retrieved November 10, 2019, from https://www.sizediversityandhealth.org/content.asp?id=152.
Image Credits:
- “Individuals with Obesity” by Obesity Canada is licensed under CC BY-ND 2.0
- Figure 7.24. Thrifty vs spendthrift genes. Fig. 1. Reinhardt, M., Thearle, M. S., Ibrahim, M., Hohenadel, M. G., Bogardus, C., Krakoff, J., & Votruba, S. B. (2015). A human thrifty phenotype associated with less weight loss during caloric restriction. Diabetes, 64(8), 2859-2867.
- Figure 7.25.“DIETFITS Study” by Journal of the American Medical Association is in the Public Domain
- Figure 7.26. “Dietary Intakes Compared to Recommendations” from Dietary Guidelines for Americans, 2020-2025, Figure 1-6 is in the Public Domain
- Figure 7.27. “Exercise Intensity” by Office of Disease Prevention and Health Promotion is in the Public Domain
- Figure 7.28. “Behavioral Weight-Loss Treatment Topics” by Heather Leonard is licensed under CC BY 4.0
- “Women Eating” by Obesity Canada is licensed under CC BY-ND 2.
- Hill JO. Can a Small-Changes Approach Help Address the Obesity Epidemic? A Report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am J Clin Nutr. 2009; 89(2), 477–84. http://www.ajcn.org/content/89/2/477.long. Accessed September 22, 2017. ↵
- Rodearmel SJ, Wyatt HR, et al. Small Changes in Dietary Sugar and Physical Activity As an Approach to Preventing Excessive Weight Gain: The America on the Move Family Study. Pediatrics. 2007; 120(4), e869–79. http://pediatrics.aappublications.org/content/120/4/e869.long. Accessed February 22, 2022. ↵
- Rodearmel SJ, Wyatt HR, et al. Small Changes in Dietary Sugar and Physical Activity As an Approach to Preventing Excessive Weight Gain: The America on the Move Family Study. Pediatrics. 2007; 120(4), e869–79. http://pediatrics.aappublications.org/content/120/4/e869.long. Accessed September 22, 2017. ↵
A hormone secreted from fat cells and signals satiety or the feeling of fullness. Therefore, it's known as the "satiety hormone" and makes us stop eating. The term is derived from the Greek word leptos, meaning thin.