Unit 7- Energy Balance and Obesity
7.4 Overweight
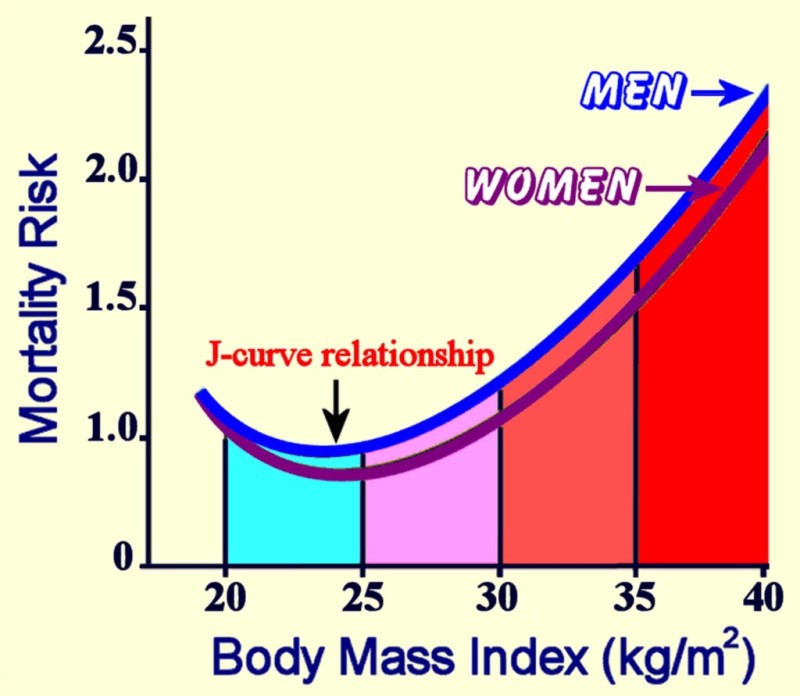
As discussed in section 7.2, energy balance is influenced by many factors. Your energy balance status ultimately influences your weight. While much of the focus in society is placed on concerns with being overweight or obese, both ends of the weight spectrum are associated with health risks. Being underweight can negatively impact health just as being overweight can. In fact, research has shown a J-shaped association between mortality risk and BMI, with greater risk for dying in underweight and obese populations and the lowest risk occuring in the normal BMI range. [1](Notice that mortality risk is greatest with BMI 35 to 40, or type III obesity.)
Figure 7.14. The relationship between body mass index and mortality forms a J-shaped curve, demonstrating higher rates of death associated with underweight and obese, with lowest rates of death associated with normal weight.
What are the specific risks associated with being overweight or underweight? Let’s take a closer look at each of these situations.
Health Risks of Being Overweight
The health consequences of too much body fat are numerous. Fat cells are not lifeless storage tanks—they’re dynamic, metabolically-active tissue that secrete a number of different hormones and hormone-like messengers, causing low-grade inflammation. These substances are believed to contribute to chronic disease development such as type 2 diabetes, cardiovascular disease, and some types of cancer.[2]
According to the World Health Organization (WHO), more people are overweight or obese than underweight. Globally, an estimated 2.8 million adults die annually as a result of being overweight or obese. [3] As BMI increases over 25, the risks increase for several health conditions, including:
- Heart disease
- Type 2 diabetes
- Hypertension
- Stroke
- Osteoarthritis
- Sleep apnea
- Some cancers (endometrial, breast, colon, kidney, gallbladder, liver)
- Depression and anxiety
- Difficulty walking, bending and climbing [4]
Childhood obesity is also a global health concern. In 2016, more than 340 million children and adolescents and 41 million preschool children were overweight or obese. And obese children are more likely to become obese adults, develop diabetes and cardiovascular disease at younger ages, and have an increased risk of premature death.
Similar to other public health organizations, the WHO states that the main causes of the global obesity epidemic are increased intake of sugary and high-fat foods and being inactive. The environmental changes that contribute to the dietary and physical activity patterns of the world today are associated with the lack of policies that address the obesity epidemic in the food and health industry, urban planning, agriculture, and education sectors.[5]

Economic and Societal Costs of Being Overweight
The economic burden of overweight and obesity has skyrocketed as obesity rates in the United States continue to climb. According to a recent report, direct health care costs due to overweight and obesity exceed $480 billion, and indirect health care costs have surpassed $1.4 trillion. (These costs are from money directly paid to treat the obesity related illnesses and lost economic productivity due to absenteeism and lost wages.) People who are obese spend about $1,500 more per year for medical care than people of healthy weight.[6]
Social and emotional consequences of being overweight or obese are no less real than economic costs. Individuals with obesity often face discrimination, lower wages, depression, anxiety, and lower quality of life. [7]
Weight bias and discrimination are of particular concern for those who are overweight or obese. Weight bias is defined as “negative weight-related attitudes, beliefs, assumptions, and judgments toward individuals who are overweight and obese,” though this bias does extend to those who are underweight as well.[8]
The incidence of weight discrimination has increased and currently occurs at rates similar to that of racial discrimination.[9] Individuals who are overweight or obese are often blamed for their disease and viewed as being lazy, stupid, ugly, and lacking in self-control or motivation.11 This bias toward people with obesity is seen in many aspects of life, including school, the workplace, health care, social events, and even the individual’s own family. [10]
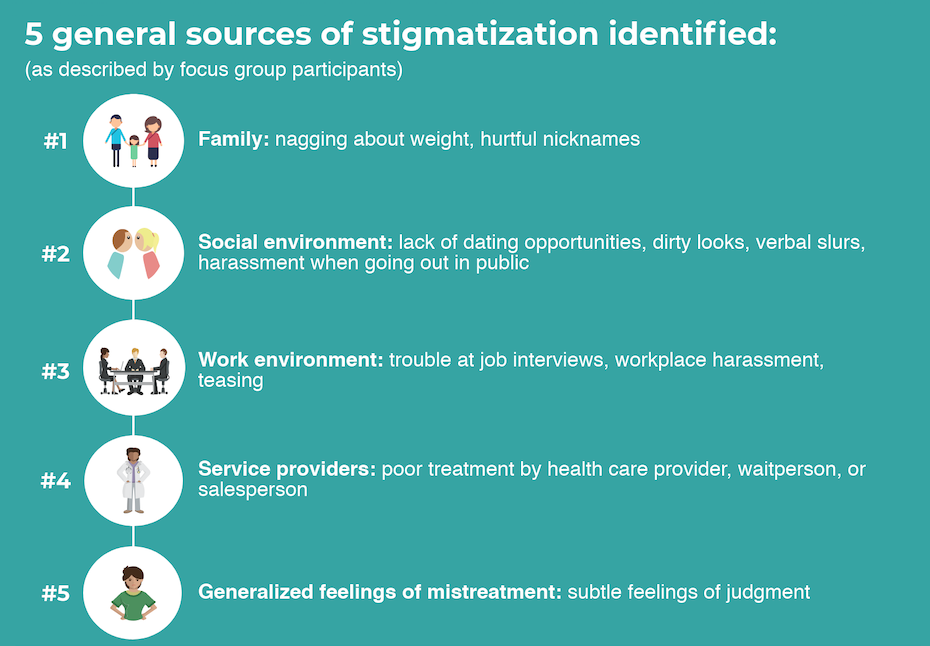
The figure below outlines the five most common sources of weight stigmatization: 1) families, 2) social environments, 3) work environments, 4) service providers, and 5) judgment from others.
Figure 7.15. Common sources of weight stigmatization identified by individuals who are overweight or obese [11]
Combatting weight bias and discrimination will require change on many levels. Changes include:
- Governments should include weight as a category covered in anti-discrimination laws.
- Schools should develop policies on harassment and bullying related to weight.
- Health care should pay for obesity treatment.
- Health care providers should be trained on weight bias awareness.
- And the public should be educated about weight bias to help change negative attitudes toward overweight and obesity.[12]
Video: “Weight of the Nation: Stigma—The Human Cost of Obesity” by HBO Docs, YouTube (May 14, 2012), 18:54. This is an excellent video to help increase awareness of weight stigma, humanizing the pain and damage caused by weight bias and discrimination.
Review Questions
Attributions:
- Lane Community College Nutrition Program, “Overweight and Underweight: What Are the Risks? ” CC BY-NC 4.0
References:
- 1Di Angelantonio, E., Bhupathiraju, S. N., Wormser, D., Gao, P., Kaptoge, S., de Gonzalez, A. B., … & Lewington, S. (2016). Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet, 388(10046), 776-786.
- 2Obesity and overweight. (2017). World Health Organization. Retrieved October 31, 2019 from https://www.who.int/features/factfiles/obesity/en/.
- 3The health effects of overweight and obesity. (2020 ). Centers for Disease Control and Prevention. Retrieved January 24, 2022, from https://www.cdc.gov/healthyweight/effects/index.html
- 4Economic impact of obesity increased to $1.4 billion. Retrieved on January 24, 2022, from https://milkeninstitute.org/article/economic-impact-obesity-increased-14-trillion-says-milken-institute
- 5. CDC. Adult Obesity Facts. Retrieved January 24, 2022, from https://www.cdc.gov/obesity/data/adult.html
- 6Obesity consequences. Harvard T.H. Chan School of Public Health. Retrieved November 4, 2019, from https://www.hsph.harvard.edu/obesity-prevention-source/obesity-consequences/economic/.
- 7Alberga, A. S., Russell-Mayhew, S., von Ranson, K. M., & McLaren, L. (2016). Weight bias: a call to action. Journal of eating disorders, 4(1), 34.
- 8Schvey, N. (2010). Weight bias in health care. AMA Journal of Ethics. Retrieved November 7, 2019, from https://journalofethics.ama-assn.org/article/weight-bias-health-care/2010-04.
- 9Understanding obesity stigma. (2019). Obesity Action Coalition. Retrieved November 7, 2019, from https://www.obesityaction.org/get-educated/public-resources/brochures-guides/understanding-obesity-stigma-brochure/.
- 10Blog, R. L., & by Age, N. The Health Impact of Weight Stigma By Carrie Dennett, MPH, RDN, CD Today’s Dietitian Vol. 20, No. 1, P. 24. Retrieved November 7, 2019, from
https://www.todaysdietitian.com/newarchives/0118p24.shtml. - 11Swinburn, B. A., Kraak, V. I., Allender, S., Atkins, V. J., Baker, P. I., Bogard, J. R., … & Ezzati, M. (2019). The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. The Lancet, 393(10173), 791-846.
- 12Weight bias: A social justice issue. UConn Rudd Center for Food Policy & Obesity. Retrieved November 4, 2019, from http://www.uconnruddcenter.org/policy-briefs-and-reports.
- Di Angelantonio, E., Bhupathiraju, S. N., Wormser, D., Gao, P., Kaptoge, S., de Gonzalez, A. B., ... & Lewington, S. (2016). Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet, 388(10046), 776-786. ↵
- Obesity and Hormones. Victoria's (Au) Better Health Channel. https://www.betterhealth. Retrieved January 25, 2022 from https://www.betterhealth.vic.gov.au/health/healthyliving/obesity-and-hormones ↵
- Obesity and overweight. (2017). World Health Organization. Retrieved October 31, 2019 from https://www.who.int/features/factfiles/obesity/en/. ↵
- Obesity and overweight. (2017). World Health Organization. Retrieved October 31, 2019 from https://www.who.int/features/factfiles/obesity/en/. ↵
- Obesity and overweight. (2017). World Health Organization. Retrieved October 31, 2019 from https://www.who.int/features/factfiles/obesity/en/. ↵
- Economic impact of obesity increased to $1.4 billion. Retrieved on January 24, 2022, from https://milkeninstitute.org/article/economic-impact-obesity-increased-14-trillion-says-milken-institute ↵
- Obesity consequences. Harvard T.H. Chan School of Public Health. Retrieved November 4, 2019, from https://www.hsph.harvard.edu/obesity-prevention-source/obesity-consequences/economic/. ↵
- Alberga, A. S., Russell-Mayhew, S., von Ranson, K. M., & McLaren, L. (2016). Weight bias: a call to action. Journal of eating disorders, 4(1), 34. ↵
- Schvey, N. (2010). Weight bias in health care. AMA Journal of Ethics. Retrieved November 7, 2019, from https://journalofethics.ama-assn.org/article/weight-bias-health-care/2010-04. ↵
- Understanding obesity stigma. (2019). Obesity Action Coalition. Retrieved November 7, 2019, from https://www.obesityaction.org/get-educated/public-resources/brochures-guides/understanding-obesity-stigma-brochure/. ↵
- Cossrow, N. H., Jeffery, R. W., & McGuire, M. T. (2001). Understanding weight stigmatization: A focus group study. Journal of nutrition education, 33(4), 208-214. ↵
- Weight bias: A social justice issue. UConn Rudd Center for Food Policy & Obesity. Retrieved November 4, 2019, from http://www.uconnruddcenter.org/policy-briefs-and-reports. ↵
A chemical messenger in the body that is released into the blood from one specific location in the body and travels to another location, where it elicits a specific response.
The body's immune system response to a stimulus, such as bacteria or viruses. Recent studies, however, show diets high in sugar and fat, or having excess body fat cause inflammation.